While many people fully recover from COVID-19 in a week or 2, some people still get symptoms weeks or months after being infected – what’s known as long COVID.
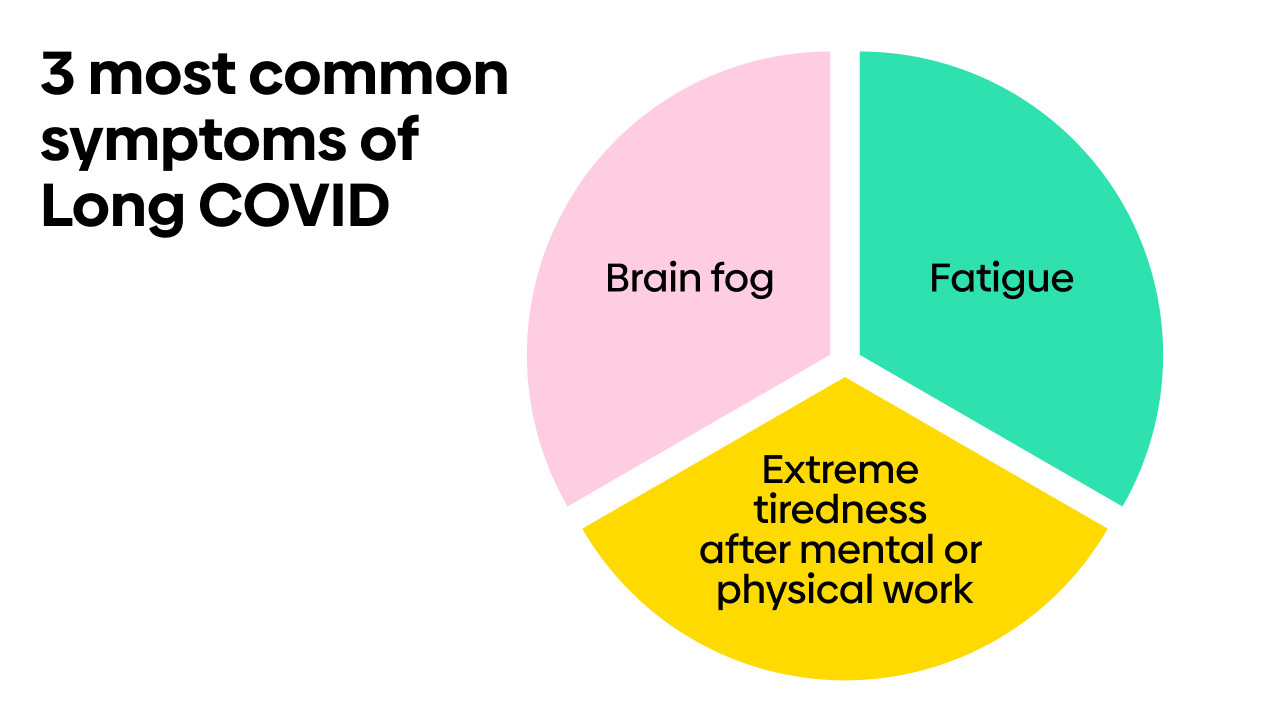
The most common long COVID symptoms include tiredness (fatigue) and shortness of breath, but research has linked the condition to hundreds of different symptoms, affecting many parts of your body. Symptoms can overlap and vary over time, too. So it’s not surprising that long COVID can be challenging to diagnose and treat.
For example, how can you tell if your brain fog and sleep problems are long COVID? They could be symptoms of the menopause instead. Equally, maybe your tummy pain is a symptom of irritable bowel syndrome (IBS), or your chest pain is a sign of angina, and not related to COVID-19 at all?
If you’re getting these sorts of symptoms, they can leave you feeling physically and mentally drained – whatever’s causing them. But there is help available. Read on to learn about how long COVID is diagnosed and what other conditions could be causing your symptoms, so you can get the right support and treatment.
How is long COVID diagnosed?
As yet, there’s no definitive test for long COVID. Instead, your doctor will use a diagnosis of exclusion – which means checking that nothing else could be causing your symptoms.
Check if you have common long COVID symptoms.
“If you develop any new or persisting symptoms after COVID-19 infection, it’s important to seek medical attention right away,” advises Dr Aleem Qureshi, GP and Healthily clinical lead. “This is to rule out any life-threatening conditions – such as blood clots, heart or lung problems – and evaluate whether your symptoms are due to long COVID or another condition.”
To do this, your doctor will take a detailed history of your physical and mental symptoms. Depending on your symptoms, they may examine you and order some tests to rule out other conditions.
Tests you may have to rule out other conditions
The tests you have will depend on your symptoms, but may include:
- blood tests – to look for signs of inflammation and check for other conditions that can cause similar symptoms, such as diabetes, thyroid problems, heart problems or kidney and liver conditions
- electrocardiogram (ECG) – to check your heart rhythm
- chest X-ray – if you’re short of breath or have a lingering cough
Your doctor may also refer you to a dedicated long COVID clinic or a specialist if they think you need other tests. More specialised tests may include:
- CT scan or MRI scan – to check your heart and lungs and rule out other causes
- tilt table test – if you’re getting dizziness and lightheadedness
- cognitive function tests – if you have memory and concentration problems (brain fog)

Long COVID and chronic fatigue syndrome (CFS)
Some of the symptoms of long COVID can be similar to those of a condition called chronic fatigue syndrome (CFS) or ME, including fatigue, brain fog and ‘post-exertional malaise’ – where your symptoms get worse after any sort of physical or mental exertion.
However, CFS is unlikely to cause symptoms such as breathlessness or chest pain, which are among the other symptoms reported in some people with long COVID.
Experts don’t know what causes CFS, but one theory is that it’s triggered by a viral infection. So far, there’s no proof that long COVID causes CFS, but researchers are looking into the link and the overlap between some symptoms, and whether they could be the same or similar conditions.
Read about how CFS/ME is diagnosed and treated.
Try these tips for managing long COVID fatigue.
Is it long COVID or the menopause?
Many symptoms of the menopause and the time leading up to it (perimenopause) also overlap with long COVID, including fatigue, brain fog, muscle and joint pain, depression, anxiety and hair loss.
But some other common menopause symptoms are less likely to be caused by long COVID, such as hot flushes, vaginal dryness, bladder problems and low sex drive (libido).
When you’re trying to work out what's causing your symptoms, it’s worth bearing in mind that long COVID is thought to be more common in women than men (read more about women and long COVID). But it’s also important that any overlap with the perimenopause or menopause isn’t overlooked.
If you’re diagnosed with menopause, there are effective treatments for these symptoms, including hormone replacement therapy (HRT). Read about self-help measures and treatments for menopause.
What else could be causing long COVID symptoms?
Because so many symptoms have been linked to long COVID, there are also lots of other things that could be causing them.
For example, joint pain can be caused by arthritis, tiredness can be due to an underactive thyroid gland, and hair loss can be caused by stress.
This is why your doctor asks for details about your symptoms and medical history. You can help them by keeping a record of your symptoms – including when they started, whether they change or come and go over time, and how they affect your daily life.
“It can be helpful to use symptom-tracking tools, such as those in the Healthily app, where you can track things like energy levels, low mood, muscle aches and sleep,” says Dr Rebecca Thomas, GP and Healthily senior clinical lead. “These general symptoms can also be present in other conditions, so tracking your symptoms to show to your doctor can be useful for making a diagnosis of long COVID, or give clues as to whether your symptoms may be caused by another condition.”
“This can be especially useful when seeing your doctor, as they will be able to understand your symptoms and how they’ve changed over time. This will help them make a diagnosis and discuss how best to support you.”
Find out what we know so far about how long symptoms of long COVID can last.
For more information about how to access support and treatment for long COVID, plus self-help tips for managing long COVID symptoms, read your long COVID treatment and recovery plan.
Your health questions answered
I was seriously ill with COVID-19 and spent 10 days in intensive care on a ventilator and several weeks in hospital recovering. Six months later, I’m still weak and have no energy – climbing stairs leaves me breathless. I have terrible brain fog, too, and can’t seem to concentrate on anything. I’m also very anxious about my health. Do I have long COVID?
Answered by: the Healthily medical team
“It’s possible that you have a combination of long COVID and a condition called post-intensive care syndrome (PICS), which is a collection of symptoms you can get after being in an intensive care unit (ICU). These can include poor concentration or memory and anxiety, as well as physical problems such as fatigue, muscle weakness and breathlessness. Symptoms can last for weeks, months or sometimes even years – your body has been through a trauma, and it takes time to recover from this. Talk to your doctor about the treatments and support available for PICS and long COVID.”







